OSHA Issues New Emergency Temporary Standard for the Healthcare Industry and Updated Guidance for General Industry

On June 10, 2021, the Occupational Health and Safety Administration (OSHA) issued its long-awaited COVID-19 Emergency Temporary Standard (ETS) for healthcare employers, along with updated guidance for other industries. Although the ETS incorporates many of OSHA and the CDC’s prior COVID-19 recommendations for healthcare settings, it creates new requirements which will serve as the basis for future enforcement. Given OSHA’s recent COVID-19 National Emphasis Program, which specifically targets the healthcare industry for inspections and enforcement, it is critical that healthcare employers update their COVID-19 policies and practices prior to enforcement of the new ETS.
COVID-19 Emergency Temporary Standard for Healthcare Services
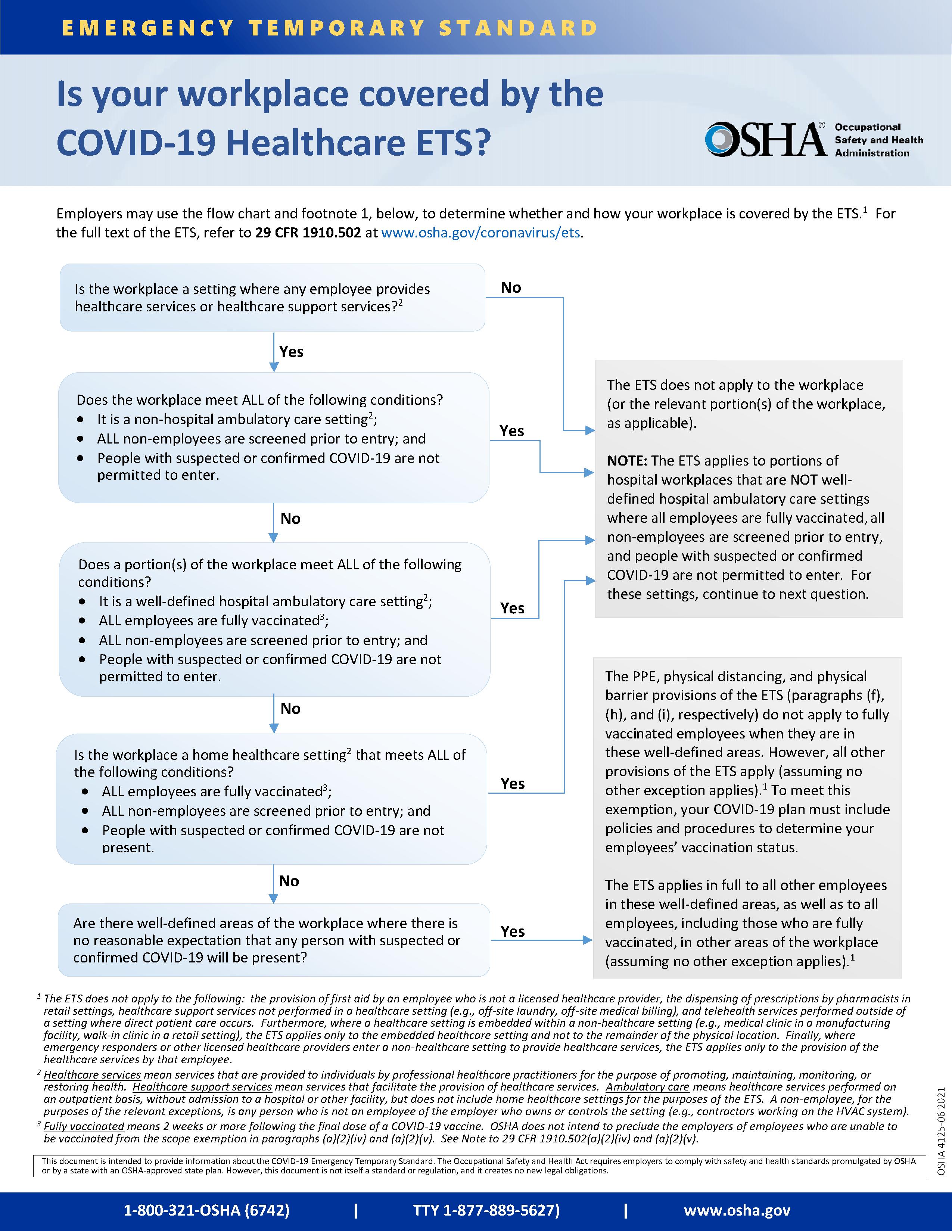 The ETS applies only to the healthcare industry and specifically targets settings where COVID-19 patients are treated such as hospitals, nursing homes, physician practices, long-term care, home health care, hospice care, emergency medical response, and dental offices. Certain healthcare settings are exempt from the new requirements to the extent that they screen and exclude non-employees with suspected or confirmed COVID-19. Where a healthcare setting is located within a non-healthcare setting, such as a medical clinic within a manufacturing facility, the ETS only applies to the healthcare setting. OSHA has published a helpful infographic to assist employers in determining whether they are subject to the ETS.
The ETS applies only to the healthcare industry and specifically targets settings where COVID-19 patients are treated such as hospitals, nursing homes, physician practices, long-term care, home health care, hospice care, emergency medical response, and dental offices. Certain healthcare settings are exempt from the new requirements to the extent that they screen and exclude non-employees with suspected or confirmed COVID-19. Where a healthcare setting is located within a non-healthcare setting, such as a medical clinic within a manufacturing facility, the ETS only applies to the healthcare setting. OSHA has published a helpful infographic to assist employers in determining whether they are subject to the ETS.
The ETS imposes the following requirements on covered healthcare providers:
- COVID-19 Plan. Healthcare employers must develop and implement a written COVID-19 plan for each workplace. Small employers with 10 or fewer employees are not required to have a written plan. Employers must designate a COVID-19 Safety Coordinator and use OSHA’s hazard assessment process to identify potential workplace hazards related to COVID-19. The COVID-19 plan must address the hazards identified by the assessment through policies, practices, and procedures designed to minimize the risk of transmission.
- Patient Screening and Monitoring. Employers must limit points of entry into the healthcare setting, and screen and triage all clients, patients, residents, delivery personal, visitors, and other non-employees upon entry. Employers may also implement other applicable patient management strategies in accordance with the CDC’s COVID-19 Infection Prevention and Control Recommendations.
- Standard Transmission-Based Precautions. Healthcare employers must implement policies and procedures to adhere to Standard and Transmission-Based Precautions in accordance with the CDC’s Guidelines for Isolation Precautions.
- Personal Protective Equipment (PPE). Employers must provide and ensure that employees wear facemasks when indoors or when occupying a vehicle with others for work purposes. There are several exceptions to the facemask requirement, including when employees are alone or eating/drinking. Significantly, facemasks and distancing are not required for fully vaccinated employees in well-defined areas where there is no reasonable expectation that any person with suspected or confirmed COVID-19 will be present. Employers may wish to use well-defined areas where masks are not required to encourage vaccination among employees.
Employees exposed to individuals with confirmed or suspected COVID-19 must be provided a respirator and other PPE. If there is a limited supply of filtering facepiece respirators (N-95), employers are encouraged to use elastomeric respirators or powered air-purifying respirators (PAPRs). Respirators are required during aerosol-generating procedures performed on a person with confirmed or suspected COVID-19. If respirators are being provided, employers must have a written respiratory protection program as required by the Respiratory Protection Standard. - Aerosol-generating Procedures. Healthcare employers must: limit the number of employees present; perform the procedure in an existing airborne infection isolation room (AIIR), if possible; and clean and disinfect the room, equipment, and surfaces following the procedure. Installation of new AIIRs is not required.
- Physical Distancing. Employers must ensure a distance of 6 feet between employees unless distancing is not feasible for a specific activity such as hands-on medical care. Physical barriers are required in work areas other than direct patient care areas such as lobbies, check-in desks, triage, pharmacy windows, billing, etc.).
- Cleaning and Disinfection. In patient care areas and resident rooms, and for medical devices and equipment, healthcare providers must comply with the CDC’s COVID-19 Infection Prevention and Control Recommendations and Guidelines for Environmental Infection Control (pages 86-103, 147-149). In all other areas, employers must: (1) clean high-touch surfaces and equipment once a day; (2) when a person who is COVID-19 positive has been in the workplace within the past 24 hours, clean and disinfect in accordance with the CDC’s Cleaning and Disinfecting Guidance; and (3) provide alcohol-based rub that is at least 60 percent alcohol or readily accessible hand-washing facilities.
- Ventilation. Employers who own or control buildings must ensure that HVAC systems are used per manufacturer instructions, that air circulation is maximized, that air filters are rated MERV-13 or higher and replaced as necessary, and all intake ports are cleaned and maintained. Employers should consider other measures to improve ventilation in accordance with the CDC’s Ventilation Guidance. The ETS does not require the installation of new HVAC systems.
- Health Screening and Management. Healthcare employers must screen employees each workday and may conduct screening through self-monitoring. Employees must be required to promptly notify the employer when the employee: (1) is COVID-19 positive either through testing or diagnosis; (2) has been told by a licensed healthcare provider that the employee is suspected to have COVID-19; (3) is experiencing loss of taste and/or smell; or (4) is experiencing both a fever greater than 100.4 and new unexplained cough associated with shortness of breath. Employees that meet any of these criteria must be immediately removed from the workplace until they met certain return to work criteria.
Employees who are COVID-19 positive either through testing or diagnosis must remain out of work until they meet the return to work criteria set forth in the CDC’s Isolation Guidance and Return to Work Guidance. Employees who are removed from the workplace for any other reason provided in the ETS must remain out of work until they meet the CDC’s return to work criteria, or they receive a negative PCR COVID-19 test result.
The ETS also imposes new financial obligations on healthcare employers. Employees who are removed from the workplace and are able to telework must be paid the same pay and benefits the employee would have received had the employee not been absent. When an employee is not able to telework, the employer must continue to provide benefits and the same regular pay the employee would have received had the employee not been absent, up to $1,400 per week, until the employee returns to work. For employers with fewer than 500 employees, the employer must pay up to $1,400/week for the first two weeks and, beginning in the third week, the amount is reduced to two-thirds of the same regular pay the employee would have received had the employee not been absent, up to $200/day. The employer’s payment obligation is reduced by the amount of compensation an employee receives from any other source, such as a publicly or employer-funded compensation program (i.e. paid sick leave).
For employers with fewer than 500 employees, OSHA’s interpretive guidance indicates that the cost of paid leave for employees who are removed from the workplace will be offset by tax credits provided under the American Rescue Plan, which are available through September 2021. Employers with 500 or more employers are not entitled to tax credit relief but can require employees to use existing paid leave during time periods they are removed from work under the ETS.
Finally, the ETS provides for notification procedures if an employee who was not wearing a respirator is in close contact with a person who is COVID-19 positive (excluding patients).
- Vaccination. Healthcare employers must support vaccination by providing reasonable time off and paid leave for vaccination and side effects.
- Training. Covered employers must ensure that employees receive training at a literacy level and in a language they understand concerning specifically identified COVID-19 topics.
- Anti-retaliation. Employers must implement protections from retaliation.
- No Cost to Employees. The implementation of the ETS must be at no cost to employees.
- Recordkeeping. Employers with 10 or more employees must retain certain records, including COVID-19 Plans and logs of any employee COVID-19 diagnoses, regardless of whether the infection occurred at work.
- Reporting of Fatalities and Hospitalizations. Healthcare employers must continue to report fatalities within 8 hours of learning of the fatality, and hospitalizations within 24 hours of learning of the in-patient hospitalization.
The ETS will not become effective until it is formally published in the Federal Register, which is expected to occur within the next two weeks. Covered healthcare employers must comply with the ETS within fourteen (14) days of its publication, so it is vital that employers immediately review their COVID-19 plans and make any necessary updates before enforcement begins. Employers have thirty (30) days from publication to implement the requirements for physical barriers, ventilation and training. Members of Post & Schell’s Health Care and Employment and Labor Practice Groups are available to assist you in implementing the ETS.
Updated Guidance for General Industry
In addition to the ETS, OSHA also updated its guidance for general industry employers titled Protecting Workers: Guidance on Mitigation and Preventing the Spread of COVID-19 in the Workplace. In light of rising vaccination rates, the updated Guidance focuses specifically on protections for unvaccinated and otherwise at-risk workers and recommends the following protective measures:
- Granting paid time off for employees to get vaccinated.
- Instructing any workers who are infected, unvaccinated workers who have had close contact with someone who tested positive for COVID-19, and all workers with COVID-19 symptoms, to stay home from work.
- Implementing physical distancing for unvaccinated and at-risk workers in communal work areas.
- Providing unvaccinated and at-risk workers with face coverings or surgical masks unless their work task requires a respirator or other PPE.
- Educating and training workers on the employer’s COVID-19 policies and procedures using formats and languages they understand.
- Suggesting that unvaccinated customers, visitors, or guests wear face coverings.
- Maintaining ventilation systems.
- Performing routine cleaning and disinfection.
- Recording and reporting COVID-19 infections and deaths in accordance with OSHA requirements.
- Implementing protections from retaliation.
- Following other applicable mandatory OSHA standards, including, but not limited to, requirements for PPE, respiratory protection, sanitation, protection from bloodborne pathogens, access to medical and exposure records.
As the number of vaccinated individuals continues to rise and legal requirements loosen, employers will need to assess their workplaces and decide what measures continue to be necessary for the protection of workers, customers, and clients. Employers should review their COVID-19 policies on a regular basis and make adjustments as needed. Employers should also be mindful of the Occupational Safety and Health requirement that employers furnish to each worker “employment and a place of employment, which are free from recognized hazards that are causing or are likely to cause death or serious physical harm.”
Post & Schell’s Employment and Labor Practice Group is available to assist you in reviewing and modifying your COVID-19 workplace plans.
Disclaimer: This post does not offer specific legal advice, nor does it create an attorney-client relationship. You should not reach any legal conclusions based on the information contained in this post without first seeking the advice of counsel.